Depending on the size, number and location of your fibroids, your surgeon may choose one of three surgical approaches to myomectomy.
Abdominal myomectomy
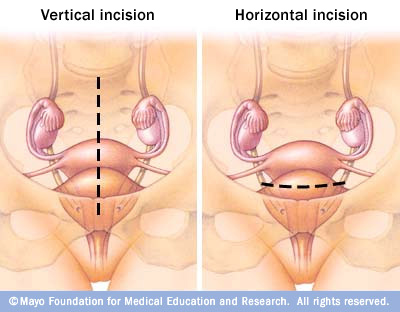
In abdominal myomectomy (laparotomy), your surgeon makes an open abdominal incision to access your uterus and remove fibroids. Your surgeon enters the pelvic cavity through one of two incisions:
-
A horizontal bikini-line incision that runs about an inch (about 2.5 centimeters) above your pubic bone. This incision follows your natural skin lines, so it usually results in a thinner scar and causes less pain than a vertical incision does. It may be only 3 to 4 inches (8 to 10 centimeters), but may be much longer. Because it limits the surgeon's access to your pelvic cavity, a bikini-line incision may not be appropriate if you have a large fibroid.
-
A vertical incision that starts in the middle of your abdomen and extends from just below your navel to just above your pubic bone. This gives your surgeon greater access to your uterus than a horizontal incision does and it reduces bleeding. It's rarely used, unless your uterus is so big that it extends up past your navel.
Laparoscopic or robotic myomectomy
In laparoscopic or robotic myomectomy, minimally invasive procedures, your surgeon accesses and removes fibroids through several small abdominal incisions.
During laparoscopic myomectomy, your surgeon makes a small incision in or near your bellybutton. Then he or she inserts a laparoscope — a narrow tube fitted with a camera — into your abdomen. Your surgeon performs the surgery with instruments inserted through other small incisions in your abdominal wall. During robotic myomectomy, instruments are inserted through similar small incisions, and the surgeon controls movement of instruments from a separate console.
The fibroid is cut into smaller pieces and removed through these small incisions in the abdominal wall or, rarely, through an incision in your vagina (colpotomy).
Laparoscopic and robotic surgery use smaller incisions than a laparotomy does. This means you may have less pain, lose less blood and return to normal activities more quickly than with a laparotomy. Uterine size and fibroid number and location are factors in determining when laparoscopic surgery is appropriate.
Hysteroscopic myomectomy
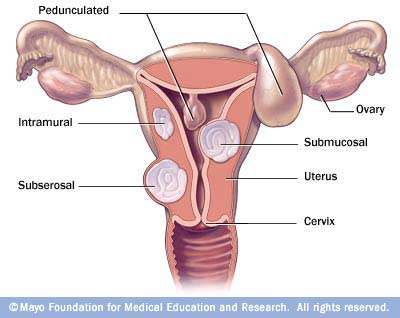
To treat fibroids that bulge significantly into your uterine cavity (submucosal fibroids), your surgeon may suggest a hysteroscopic myomectomy. Your surgeon accesses and removes fibroids using instruments inserted through your vagina and cervix into your uterus.
Your surgeon inserts a small, lighted instrument — called a resectoscope because it cuts (resects) tissue using electricity or a laser beam — through your vagina and cervix and into your uterus. A clear liquid, usually a sterile salt solution, is inserted into your uterus to expand your uterine cavity and allow examination of the uterine walls. Using the resectoscope, your surgeon then shaves pieces from the fibroid until it aligns with the surface of your uterine cavity. The removed tissue washes out with the clear liquid that's used to expand your uterus during the procedure.
Rarely, surgeons also use a laparoscope inserted through a small incision in your abdomen to view the pelvic organs and monitor the outside of the uterus during a complicated hysteroscopic myomectomy.
When you go home
At discharge from the hospital, your doctor prescribes oral pain medication, tells you how to care for yourself, and discusses restrictions on your diet and activities.
You may have to avoid certain activities, such as driving, lifting heavy objects, climbing stairs or exercising vigorously until you recover. Also, your doctor may advise that you not use tampons or have sexual intercourse during recovery. You can expect some vaginal spotting or staining for a few days up to six weeks, depending on the type of procedure you've had.
-
Abdominal myomectomy recovery typically takes four to six weeks.
-
Laparoscopic or robotic myomectomy recovery typically takes two to three weeks.
-
Hysteroscopic myomectomy recovery typically takes less than a week.